Particularly pronounced among individuals who converted to full-blown illness
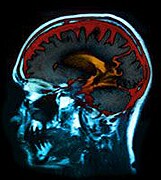
WEDNESDAY, Aug. 12, 2015 (HealthDay News) — Among individuals at clinical high risk for psychosis, thalamic dysconnectivity is evident, according to a study published online Aug. 12 in JAMA Psychiatry.
In a multicenter, two-year follow-up case-control study, Alan Anticevic, Ph.D., from the Yale University School of Medicine in New Haven, Conn., and colleagues examined whether thalamocortical connectivity is altered in individuals at risk for psychosis. Data were included for 243 individuals at clinical high risk of psychosis, of whom 21 converted to full-blown illness, and 154 healthy controls (all aged 12 to 35 years).
The researchers identified thalamocortical dysconnectivity among individuals at clinical high risk for psychosis, which was particularly pronounced in the participants who converted to full-blown illness. Widespread hypoconnectivity was seen between the thalamus and prefrontal and cerebellar areas; the pattern was more prominent among those who converted to full-blown illness. Marked thalamic hyperconnectivity was seen in sensory motor areas, which was also most pronounced among those who converted to full-blown illness. Significant correlations were seen for both patterns with concurrent prodromal symptom severity.
“Dysconnectivity correlated with symptom severity, supporting the idea that thalamic connectivity may have prognostic implications for risk of conversion to full-blown illness,” the authors write.
Copyright © 2015 HealthDay. All rights reserved.