In both therapies, stem cells are removed from a patient’s blood for treatment
By Physician’s Briefing Staff HealthDay Reporter
FRIDAY, Dec. 8, 2023 (HealthDay News) — Two milestone gene therapies for sickle cell disease have been approved by the U.S. Food and Drug Administration.
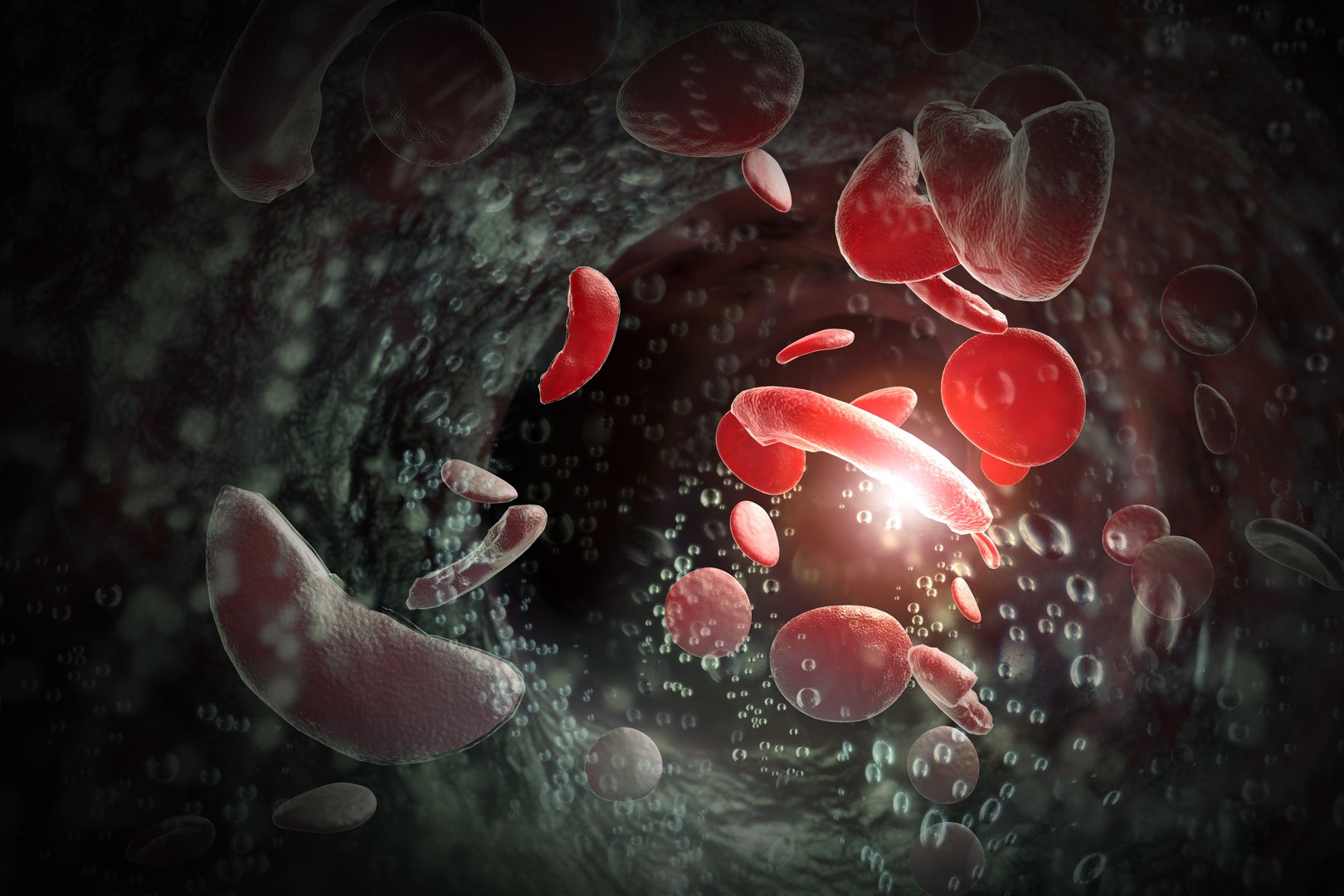
Casgevy is the first medicine available in the United States to treat a genetic disease using the CRISPR gene-editing technique. The one-time treatment permanently changes DNA in a patient’s blood cells, freeing them from the excruciating symptoms of sickle cell disease for life. The other approved therapy, Lyfgenia, uses a common virus to deliver genetic modifications to a patient’s blood stem cells in their bone marrow.
In both therapies, stem cells are removed from a patient’s blood for treatment. With Casgevy, CRISPR gene-editing technology knocks out a gene that triggers the development of defective, crescent-shaped blood cells. Meanwhile, medicine kills off flawed blood-producing cells in patients, who are then given back their own altered stem cells. The same thing happens with Lyfgenia, only a virus is used to deliver a genetic payload that causes the blood cells to start producing healthy hemoglobin. The genetically modified blood stem cells are then given back to the patient as a one-time, single-dose infusion.
Evidence supporting the approval of Casgevy was from a study of 44 patients treated with the gene-editing process. Out of 31 patients with sufficient follow-up time to be evaluated, 29 had complete freedom from the severe pain and organ damage that can occur during a sickle cell exacerbation. Furthermore, no patients experienced graft failure or graft rejection. Approval of Lyfgenia was supported by a 24-month study in which 32 patients received the therapy. Of those, 28 had no sickle cell events following their transplant.
Approval of Casgevy and Lyfgenia was granted to Vertex Pharmaceuticals and Bluebird Bio, respectively.
Copyright © 2023 HealthDay. All rights reserved.