The 65th Annual Meeting of the American Society for Radiation Oncology
By Beth Gilbert HealthDay Reporter
The annual meeting of the American Society for Radiation Oncology was held from Oct. 1 to 4 in San Diego and attracted approximately 11,000 participants from around the world, including physicians, oncology nurses, radiation therapists, biologists, physicists, and other cancer researchers. The conference featured educational courses focusing on radiation, surgical, and medical oncology.
In one study, Kathy Han, M.D., of the Princess Margaret Cancer Center at the University of Toronto, and colleagues found that liquid biopsy tests looking at persistent human papillomavirus (HPV) circulating tumor DNA (ctDNA) following chemoradiotherapy (CRT) can accurately identify inferior progression-free survival in patients with cervical cancer.
The authors assessed two liquid biopsy assays, including a digital polymerase chain reaction test and a sequencing-based assay (HPV-seq) that enables highly sensitive detection and accurate HPV genotyping from baseline plasma cell-free DNA, the main cause of cervical cancer. Seventy patients from four centers who were diagnosed with HPV-positive cervical cancer and treated with CRT were enrolled in the study and followed for just over two years. Patients provided blood samples at three time points. The researchers found that both tests were equally effective in identifying minimal residual disease among patients with cervical cancer who completed CRT. In addition, detectable HPV ctDNA at each of the three time points (end of CRT; four to six weeks after CRT; and three months after CRT) was independently associated with inferior progression-free survival.
“HPV ctDNA testing can identify, as early as at the end of CRT, cervical cancer patients at high risk of recurrence or future treatment intensification trials,” Han said.
Several authors disclosed pending patents related to HPV ctDNA (HPV-seq).
As part of the FABREC study, Julia Wong, M.D., of the Dana-Farber Brigham Cancer Center in Boston, and colleagues found that patients with breast cancer who undergo implant-based reconstruction immediately following mastectomy and receive a shorter course of radiation therapy experience similar outcomes to patients who receive a conventional course of radiation.
The authors randomly assigned 400 patients to a short course (three weeks) or conventional course (five weeks) of radiation after mastectomy with immediate implant-based reconstruction. The researchers found that patients receiving the short course and those receiving the conventional course of radiation therapy experienced comparable outcomes. Specifically, the primary outcome measure — change in physical well-being (PWB) at six months — was similar. In addition, toxicity and cancer outcomes were similar. Among younger patients, PWB was better among those who received the short course of radiation. The short-course group experienced fewer unpaid hours of time off work for treatment as well as fewer treatment breaks.
“Patients who have often gone through months of treatment prior to radiation, can safely undergo three instead of five weeks of postmastectomy radiation and have similar outcomes,” Wong said.
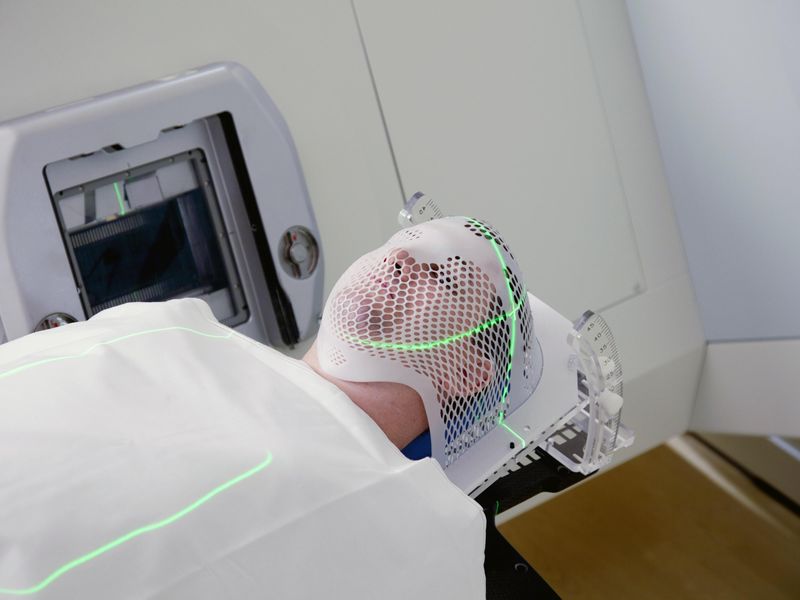
In the multi-institutional phase II study TransTasman Radiation Oncology Group FASTRACK II, Shankar Siva, Ph.D., of the Peter MacCallum Cancer Centre and the University of Melbourne in Australia, and colleagues found that high-dose radiation is an effective treatment option for older patients with kidney cancer who are ineligible for surgery.
FASTRACK II is the first multicenter clinical trial of a nonoperative therapy for patients with primary kidney cancer. In this study, the authors enrolled patients who were unable or unwilling to undergo surgery and tested a novel therapy — stereotactic ablative body radiotherapy (SABR) — as a curative treatment option. Patients received either one or three SABR treatments. After an average follow-up of 43 months, the researchers noted a low rate of side effects associated with the treatment, which provided unprecedented efficacy. The investigators observed 100 percent local control and 100 percent cancer-specific survival. In other words, no patient failed the treatment and no patient died from the treatment.
“The influence on clinical practice, I suspect, will be wide, given the adoption of this technique, and we are hoping that in the future we can conduct a randomized controlled trial of surgery versus SABR for clearly operable patients to determine which is the best option,” Siva said. “I think if patients were given the choice, they would probably opt for a totally noninvasive treatment like SABR.”
ASTRO: Shorter Radiation Feasible for Low-, Intermediate-Risk Prostate Cancer
MONDAY, Oct. 16, 2023 (HealthDay News) — At five years, five-fraction stereotactic body radiotherapy is noninferior to control radiotherapy for biochemical/clinical failure in men with localized prostate cancer, according to a study presented at the annual meeting of the American Society for Radiation Oncology, held from Oct. 1 to 4 in San Diego.
Read Full Text
ASTRO: Hypofractionation Effective for Radiotherapy After Breast Reconstruction
For women undergoing implant-based breast reconstruction after a mastectomy, use of shorter radiotherapy courses (hypofractionation) is as effective as conventionally fractionated radiotherapy, according to a study presented at the annual meeting of the American Society for Radiation Oncology, held from Oct. 1 to 4 in San Diego.
Read Full Text
ASTRO: Liquid Biopsy Can Stratify Risk in Oligometastatic NSCLC
WEDNESDAY, Oct. 11, 2023 (HealthDay News) — Liquid biopsy, which identifies circulating tumor DNA, performed before radiotherapy can stratify risk for oligometastatic non-small cell lung cancer patients, according to a study published online Oct. 2 in npj Precision Oncology to coincide with the annual meeting of the American Society for Radiation Oncology, held from Oct. 1 to 4 in San Diego.
Read Full Text
Copyright © 2023 HealthDay. All rights reserved.